Book Description
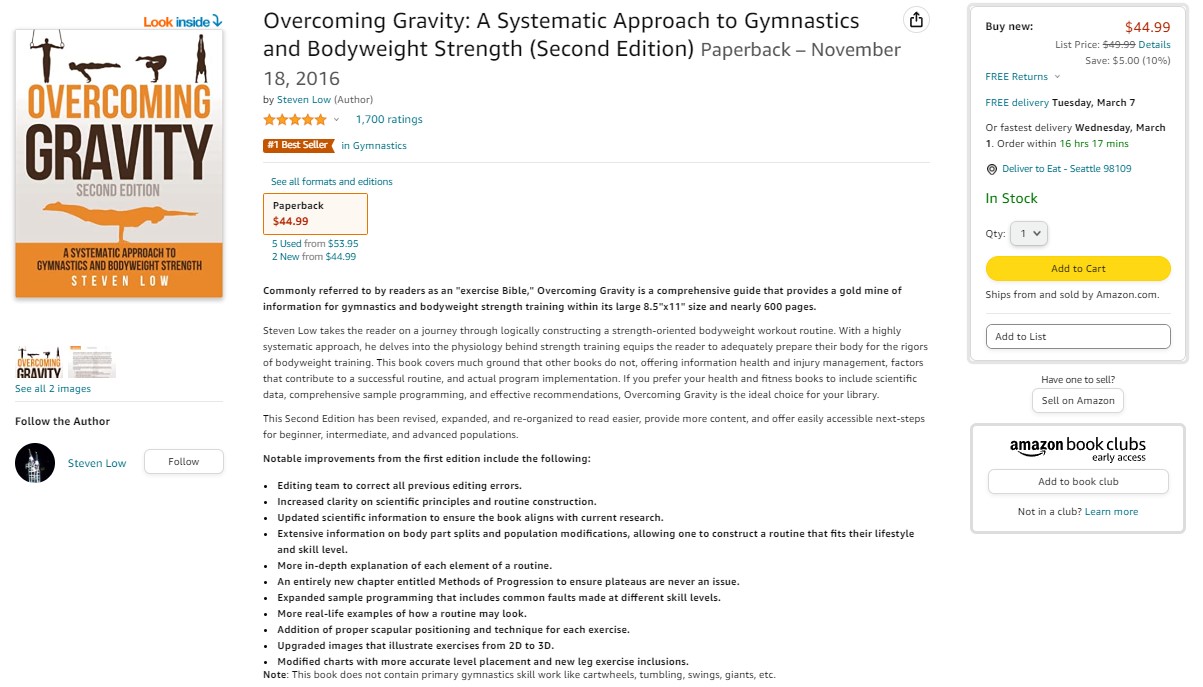
Commonly referred to by readers as an “exercise Bible,” Overcoming Gravity is a comprehensive guide that provides a gold mine of information for gymnastics and bodyweight strength training within its nearly 600 pages.
Buy Overcoming Gravity 2nd Ed Physical Book on Amazon or Digital Edition in the store.
Steven Low, who holds a BS in Biochemistry and a Doctor of Physical Therapy from the University of Maryland, takes the reader on a journey through logically constructing a strength-oriented bodyweight workout routine. With a highly systematic approach, he delves into the physiology behind strength training and equips the reader to adequately prepare their body for the rigors of bodyweight training. This book covers much ground that other books do not, offering information on health and injury management, factors that contribute to a successful routine, and actual program implementation. If you prefer your health and fitness books to include scientific data, comprehensive sample programming, and effective recommendations, Overcoming Gravity is the ideal choice for your library.
This Second Edition has been revised, expanded, and re-organized to read easier, provide more content, and offer easily accessible next-steps for beginner, intermediate, and advanced populations. Notable improvements include the following:
- Increased clarity on scientific principles and routine construction.
- Updated scientific information to ensure the book aligns with current research.
- Extensive information on body part splits and population modifications, allowing one to construct a routine that fits their lifestyle and skill level.
- More in-depth explanation of each element of a routine.
- An entirely new chapter entitled Methods of Progression to ensure plateaus are never an issue.
- Expanded sample programming that includes common faults made at different skill levels.
- More real-life examples of how a routine may look.
- Addition of proper scapular positioning and technique for each exercise.
- Upgraded images that illustrate exercises from 2D to 3D.
- Modified charts with more accurate level placement and new leg exercise inclusions.
Note: This book does not contain primary gymnastics skill work like cartwheels, tumbling, swings, giants, etc.
Overcoming Gravity Charts and Preview Content
Overcoming Gravity Second Edition charts were primarily constructed off of the Federation [of] International Gymnastics Code of Points — often referred to as the FIG COP — which is the categorical ranking of value of elements within gymnastics routines that you see on television every Olympics. Yes, you will be working toward some of the elements that gymnasts may perform in the Olympics, but that is a long road of progression! If you are interested, you can see a sample of the FIG COP for Mens Artistic Gymnastics for the 2017-2020 quadrennium.
These charts, combined with Methods of Progression in Chapter 10, will help you progress through the various levels until you can perform movements like handstands, hanstand pushups, planche, front lever, back lever, elbow levers, and many other movements to show off your strength and skill.
- Charts: Overcoming Gravity 2’s (OG2) Charts: Google Document and Print PDF (w/o abbreviations).
- Preview: Table of Contents, Introduction, Chapters 1, 2, and most of 3
Questions and Answers
Question: Is the First Edition required for purchasing the Second Edition?
Answer: No, the Second Edition is stand alone. If I were rating the clarity and depth of content, the first book was 5/10 for beginners and 7/10 for intermediate and advanced. The second book is 9+/10 for beginners, intermediate, and advanced.
Question: If I have the First Edition, should I buy the Second Edition?
Answer: The Second Edition is not your average college textbook that sees a few changes and is published again. The book was expanded from about 165,000 words to about 250,000 words, some injury content was dropped, and I added a ton of new material. Everyone who has bought the second edition and had the first edition has told me that they were more than satisfied with the quality and amount of extra content added.
Question: Is the physical book only available on Amazon?
Answer: It is only available on Amazon and a select few climbing gyms. The Digital edition (PDF/ePUB) is available here.

Buy Overcoming Gravity 2nd Ed Physical Book on Amazon or Digital Edition today!
Why Buy Overcoming Gravity?
The Overcoming Gravity: A Systematic Approach to Gymnastics and Bodyweight Strength (Second Edition) has been vastly expanded from the First Edition’s 542 pages to the Second Edition’s 598 pages. Nearly 50% more content was packed into the book word, which went from a word content of 165,000 to nearly 250,000. I also removed large portions of redundant content and specialized content on injuries from the First Edition, and greatly expanded the foundation knowledge and explanations on everything from routine construction, to health and injury management, and exercise technique in the Second Edition. All of this was to help you, the reader, understand all of the fundamental aspects of gymnastics and bodyweight strength training.
Overcoming Gravity Second Edition was written for the beginner, intermediate and advanced in mind. The main goal of the book is bodyweight strength training education in the vein of the common proverb:
“Give a man a fish and you feed him for a day; teach a man to fish and you feed him for a lifetime.”
In other words, the goal of the book is to provide you, the reader, information on gymnastics and bodyweight strength training that will last you an entire lifetime.
The majority of books on strength and conditioning and bodyweight training lay out a training program for the you to follow. While these training programs can be effective, they all have inherent limitations to them. The most common problem with formatted programs is that they are often “cookie cutter.” These programs are designed for a large portion of the population, but they often do not have appropriate modifications for those with special needs. Overcoming Gravity addresses many of these specific needs by discussing modifications that can be made to the program such as if you are sedentary versus active, young versus old, into sports-specific or recreational training, and even uninjured or injured.
Likewise, Overcoming Gravity Second Edition looks at the planning of routines — often called periodization — through the lens of progress. What changes to a routine can be made in order to make safe and effective progress for the beginner, intermediate, and advanced. Routines are too often constructed solely get you engaged with exercise. The focus on progress will ultimately help you get to the goals that you desire, whether it be the gymnastics isometrics, strength movements, hypertrophy, and a healthy body. This is done by engaging you, the reader, with the information about routine implementation (full body routine and splits) and how to fit skill work, strength work, flexibility, and prehabilitation together. This allows the user to create an effective routine that is optimized toward their goals

Chapter 10: Methods of Progression is one of the big additions to Overcoming Gravity Second Edition. This chapter was not in the previous edition and is also the first of its kind in any gymnastics, bodyweight, or calisthenics product. This section was designed to educate you on the methods of progress for bodyweight exercises. Barbell and Dumbell exercises are very easy to know how to progress: simply add weight. However, bodyweight exercises are very difficult to understand how to progress safely and effectively. It is simply more than just adding repetitions until you can reach the next progression.
The third part of the book discusses various factors that influence training such as endurance, cardio, cross training, hybrid templates, and routines. It also discusses factors such as overreaching, overtraining, health and injury management, and lifestyle factors such as optimizing sleep, nutrition, and stress for your goals. All of these factors are important to understand how they influence your training, especially if you are going to add or subtract elements from your routine. Most fitness books may sparsely mention these things here and there, but Overcoming Gravity Second Edition makes you aware of everything that can influence how you progress and perform.
Part four of the book discusses program implementation giving sample routines, real life examples, and commentary about common pitfalls that beginners, intermediates, and advanced may run into in their training. This section is not so you can go about copying the routines that have been constructed or others have used in the past. However, it is there to give you a reference and structure on how routines can be built and managed during a cycle, so that you can take what you have learned and implement it well.
Finally, the fifth part of the book is everything to do with keeping your body health and exercise. The first part of this section is about common bodyweight training injuries to make you aware of factors that can derail your training. Likewise, the prehabilitation, mobility, and flexibility section gives illustrated examples of these attributes for the wrists, elbows, shoulders, core, and legs. This allows you to combine these elements into your routine along with your strength work to ensure that you are building the requirements to make it to the next level. The last part of this section is about all of the handstand, pulling, pushing, and combined exercise progressions that you need to work toward high level strength.
Overcoming Gravity Online series
I’ve started the Overcoming Gravity Online video series on Youtube as a supplement for the book, or if you don’t have it then it can be a great introduction to the book.
One of the best parts of the book is the support from the community. Overcoming Gravity Second Edition has its own subreddit on /r/overcominggravity and is one of the most highly rated training materials in /r/bodyweightfitness, which is the largest gathering of bodyweight enthusiasts in the world at over 3,400,000 users. If you want to discuss the material from Overcoming Gravity, post up a training routine for critique, get an exercise technique critique, or simply discuss bodyweight training with like-minded users, you can do all of it! I personally check /r/overcominggravity to help users understand and apply the material through questions and routines, and I also moderate bodyweightfitness as I love the bodyweight community.

Finally, here are some reviews and articles about Overcoming Gravity Second Edition:
- Gold Medal Bodies (GMB) Review
- Tykato’s video review
- Art of Manliness’ Learning a full Handstand from Overcoming Gravity
- Is Overcoming Gravity 2 worth buying?
The book still has over 4.8/5.0 rating with over 1,700 reviews!
Thanks for reading!
Buy Overcoming Gravity 2nd Ed Physical Book on Amazon or Digital Edition in the store!